White lung pneumonia in children indirectly results from large-scale vaccination against SARS-CoV-2
Several countries have been reporting a spike in cases of white lung pneumonia (e.g., China, the Netherlands, the UK, the USA, Denmark…). While the vaccination status of school-age children contracting white lung pneumonia (WLP) is rarely reported, it is highly improbable that these cases are linked to COVID-19 (C-19) vaccination. This is because vaccination rates in this age group remain very low. It is also highly unlikely that the lifting of previous restrictions on social interactions contributed to the spike in cases, as variants circulating since the advent of Omicron are highly infectious and often transmitted asymptomatically. The fact that WLP is not only reported in China, but in several other countries shows that previous confinement policies no longer have any impact on the landscape of currently circulating SARS-CoV-2 (SC-2) variants.
The reason why WLP predominantly (but not exclusively) affects children aged 5 to 12 is that, at this stage, they have not yet transitioned from natural/innate antibody(Ab)-mediated protection against glycosylated components[1] to trained, cell-mediated innate immunity[2]. This plays a crucial role in the putative pathogenesis outlined below.
WLP shares similarities with MIS-C (multisystemic inflammatory syndrome in children), observed in children of the same age group (5-12 years), often following a previous mild infection (https://www.voiceforscienceandsolidarity.org/scientific-blog/mis-c-in-children-does-not-justify-at-all-their-vaccination-against-sars-cov-2). Similar to MIS-C, WLP is a post-infectious inflammatory condition resulting from heightened viral infectivity.
In the case of MIS-C, this enhanced infectivity is due to infection-enhancing anti-S(pike) Abs generated upon re-exposure after a mild SC-2 infection. As some children are exposed to new, more infectious SC-2 variants shortly after experiencing a mild infection, the previously infection-primed anti-S Abs' neutralizing capacity proves insufficient to neutralize the new variant. Due to their significantly diminished neutralizing capacity, these Abs are believed to foster the formation of multimeric virus-Ab complexes while outcompeting the child's innate, low-affinity IgM Abs. While enhanced viral infectiousness, combined with sidelined innate Abs, occasionally led to systemic inflammatory disease (i.e., 'multi-systemic' inflammation), severe C-19 disease was averted due to the infection-enhancing non-neutralizing Abs (NNAbs), which mitigate viral virulence (https://braintrain.mykajabi.com/the-inescapable-immune-escape-pandemic).
The enhanced infectivity of SC-2 likely underlying WLP is attributed to the high intrinsic infectiousness of circulating Omicron descendants, while neutralizing Abs (NAbs) produced in response to a mild infection outcompete the child’s innate, low-affinity IgM Abs. The combined impact of increased intrinsic infectiousness and the sidelining of innate Abs occurs at a stage when the child’s natural killer (NK) cells are still predominantly 'pathogen-inexperienced.' It is reasonable to assume that this combined impact renders some previously infected children susceptible to breakthrough infections (BTIs), subsequently promoting the formation of multimeric complexes between the progeny virus and poorly neutralizing, previously infection-primed Abs. As explained earlier, these multimeric virus-Ab complexes stimulate the production of NNAbs, thereby protecting unvaccinated children from severe C-19 disease.
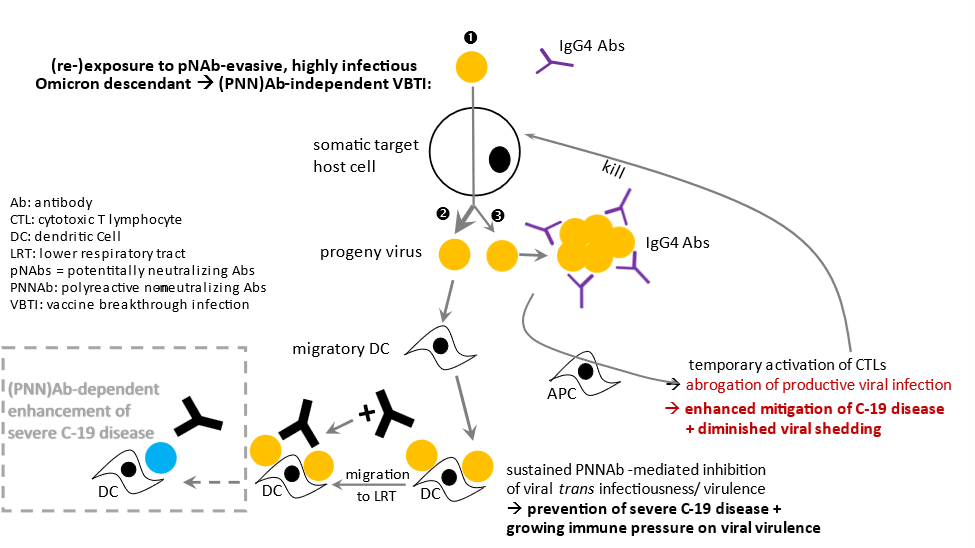
I previously described how dendritic cells (DCs) patrolling the upper respiratory tract (URT) may migrate to the lung after encountering highly infectious SC-2 in the URT. Highly infectious variants provoke an overall immune environment that is unfavorable to antigen uptake by DCs, thereby hindering the maturation of DCs and their migration to the local draining lymph nodes. Instead, highly infectious SC-2 virions adsorb to the surface of these DCs when causing BTI in the URT (see fig. attached below). Although NNAbs[3] elicited upon immune system stimulation by complexes of progeny virus and Abs with strongly diminished neutralizing capacity prevent the transfer of these highly infectious SC-2 variants to susceptible lung cells, massive migration of virus-tethered DCs to the lung likely triggers extensive inflammation, thereby promoting colonization of the lungs with commonly circulating pneumotropic pathogens (see below).
The pathogenesis explained above suggests that enhanced microbial infection is not the cause but rather secondary to pulmonary inflammation. I therefore prefer to refer to this condition as white lung syndrome (WLS) rather than WLP. All individuals whose innate immune response towards glycosylated viruses has been sidelined and possess Abs with strongly diminished neutralizing capacity could, therefore, become susceptible to WLP. I therefore tend to believe that, besides children, this disease could also affect C-19 vaccinees, particularly those who have not yet developed sufficiently strong CTL (cytotoxic T lymphocyte) activity to eliminate highly infectious progeny virus before it massively adsorbs onto URT-resident DCs.
As the sidelining of cell-based innate immunity would impact protection against glycosylated microorganisms, it is not surprising that enhanced lung inflammation is associated with colonization of the lower respiratory tract by Mycoplasma pneumoniae, RSV, Influenza or even Streptococcus pneumoniae. Since there are no human vaccines for these airborne pathogens (e.g., Mycoplasma pneumoniae and RSV in children), or as children are not vaccinated against Influenza, the immune defense against these pathogens largely depends on short-lived pre-existing Abs (only in case of previous infection) and/ or innate immunity.
Based on the putative mechanism of pathogenesis, I postulate that, similar to MIS-C, the wave of inflammatory lung disease will be short-lived. As the pandemic evolves and more infectious EG.5 or BA2.86 descendants start dominating the scene, I anticipate a rapid fall in the number and severity of WLS cases. The reason is that when viral infectiousness increases, more children will become re-exposed to a circulating variant at an earlier stage in life, i.e., at a timepoint where their innate Ab titers are high enough to cope with the highly infectious circulating variants, thus decreasing the risk of symptomatic infection. More children will , therefore, develop asymptomatic infections and be unlikely to see their innate Ab capacity dramatically reduced by infection-primed S-specific NAbs. But also in vaccinees, the risk of WLP will decrease as more vaccinees are now progressing to develop enhanced CTL activity (due to an increased uptake of large virus-Ab complexes), thereby decreasing the viral load adsorbed on migratory DCs (see fig. below).
The bottom-line is that in all cases, inflammatory organ disease in unvaccinated children is caused by enhanced viral infectivity, either due to Ab-dependent enhancement of infection or enhanced intrinsic infectiousness of circulating variants. In both scenarios, the higher infection rate in the population (including households!) comes with an added likelihood for children to become re-infected shortly after their previous asymptomatic infection, thereby sidelining the innate immune response against airborne glycosylated viruses.
It is crucial to understand that both the enhancement of viral infection and enhanced intrinsic viral infectiousness directly result from collective immune pressure placed on viral infectivity as a consequence of mass vaccination. This population-level immune pressure has driven natural selection and the (co-) circulation of more infectious immune escape variants.
Similar to MIS-C, WLS should resolve within a few days after timely and adequate immunosuppressive and anti-inflammatory treatment. Neither MIS-C nor WLS justifies C-19 vaccination for children, as C-19 vaccines, particularly mRNA vaccines, promote the sidelining of the child’s cell-based innate immune system.
In the context of WLS, the argument that a large-scale rollout of updated C-19 vaccines would control viral infectivity is incorrect. This is because updated C-19 vaccines, at best, boost titers of subneutralizing Abs, the low affinity of which would only contribute to increasing the collective immune selection pressure on viral infectiousness and, consequently, promote the pathogenesis of WLS in children.
Fig.: Pathogenesis of Ab-independent vaccine breakthrough infection (VBTI)BTI. High intrinsic infectiousness of co-circulating Omicron descendants precipitates infection of target host cells (1) and enhances the production rate of highly infectious progeny virus. The latter predominantly adsorbs onto tissue-resident DCs and thereby causes pre-existing PNNAbs to only bind in relatively low concentration to progeny virus tethered to migratory DCs (2). Diminished virulence-inhibiting capacity of pre-existing PNNAbs causes highly C-19 vaccinated populations to raise immune selection pressure on viral virulence while still protecting vaccinees from severe disease. Once binding of low-affinity IgG4 Abs to progeny virus results in the formation of large virus-Ab complexes, the concentration of progeny virus adsorbed to DCs will diminish and thereby reduce the risk of WLS. Instead, enhanced uptake of IgG4 Ab-virus complexes into patrolling APCs facilitates strong activation of cytotoxic T cells (CTLs) and thereby enables elimination of virus-infected host cells (3). However, deficient recall of T helper memory cells will entail a decline in PNNAb titers. As a result, PNNAb-mediated population-level immune selection pressure on viral virulence will gradually increase upon subsequent VBTIs caused by circulating, highly infectious variants. Dominant circulation of immune escape variants with an ever-increasing intrinsic infectiousness will ultimately cause the highly C-19 vaccinated population to raise the immune selection pressure on viral virulence beyond the threshold triggering selection of new, highly virulent variants that enable large-scale occurrence of PNNAb-dependent enhancement of severe disease (ADESD). Individuals in whom a significant portion of highly infectious progeny virions are adsorbed to DCs, rather than being complexed by IgG4 Abs to form aggregates that are subsequently taken up by APCs, are considered at risk of developing WLS.
(source: https://www.voiceforscienceandsolidarity.org/scientific-blog/the-emergence-of-a-highly-virulent-variant-is-inescapable).
Footnotes:
[1] Including viruses or small microorganisms containing glycosylated components in their envelope/ membrane
[2] As children grow older, they progressively replace the ‘self’-sensing innate Ab capacity by a pool of pre-primed Natural Killer cells that can recognize pathogen-derived self-mimicking (i.e., ‘altered self’) motifs on virus-infected or otherwise pathologically altered host cells such as to kill those cells.




Dr Geert
Today in CDC’s weekly update
https://www.cbsnews.com/news/covid-variant-jn1-flu-surge-hospitals-cdc-warns/
they reported a steady rise in MIS-C since the summer as well as pediatric hospital beds at near capacity. Though they blame the causative factor as being “covid 19”, not the mechanism of the highly infectious variants and the sidelined innate immune system overhhelming the childrens immune capacity, thereby making them more susceptible to secondary immune pathology and infections (including RSV, flu and bacterial ). After gaining a more detailed understanding of your views and projections in your latest course, I have to concur that we are (unfortuantely) seeing it evolve in real time, like a scary Hollywood movie.
I think the difficulty now too is that since your warnings/writings have been largely ignored to date, it is a tall order for most people including scientists and public health “authorities” to sit down and methodically comb through your writings with the “mental stamina” (your phrase) that is needed to really grasp the meaning and nuance of your work; Especially when things are unraveling so quickly as you have been saying for a long time.
Much gratitude for your perseverance and scholarship
Anthony
Thank you for sharing that analysis. Is there anything we can/should do about our children to avoid severe lung problems ? Just keeping them to update immunity all the time with newer variants is enough or should we avoid reinfections till abs mature ? It looks a bit scary and even now some hospitals in EU for example start to be not widely available. We know that things can get bad and we love our children so much that as an parent would like to do everything possible.