Failure to study the adaptive immune dynamics following mass Covid-19 vaccination leads scientists to point to immunocompromised patients as a potential breeding ground for highly mutated SARS-CoV-2 v
A recent article in SALON (https://www.salon.com/2024/01/12/more-severe-disease-symptoms/) cites two publications where researchers report their findings that currently emerging and predominating variants can infect lung cells more efficiently (https://pubmed.ncbi.nlm.nih.gov/38194966/; https://pubmed.ncbi.nlm.nih.gov/37745517/).
I am appalled by how the scientific community continues to mislead the public regarding the potential harm that the current evolution of SARS-CoV-2 (SC-2) towards more pneumotropic variants could inflict on highly Covid-19 (C-19) vaccinated populations.
First, the authors’ assessments are either based on in vitro analysis of altered biological traits exhibited by pseudotyped particles or in vitro analysis of productive viral infectivity measured by plaque-forming units on TMPRSS2 (transmembrane protease serine 2)-negative Vero cells (instead of on TMPRSS2-positive lung cells). Considering the pivotal role played by BA.2.86/ JN.1 viral proteins, other than the Spike (S) protein, in enhancing the productive infectiousness of these variants, any in vitro evaluation of viral infectivity based on the analysis of cell entry by pseudotyped particles may not be relevant to in vivo viral transmissibility. Additionally, due to the TMPRSS2-dependent pathway of BA2.86 for viral entry through plasma membrane fusion, assessments of viral infectivity involving the inoculation of viral progeny on TMPRSS2-negative Vero cells may not be representative of the in vivo scenario. Moreover, given the crucial function of polymeric, non-neutralizing antibodies (PNNAbs) in attenuating viral trans infection and trans fusion activity displayed by Omicron descendants, any in vitro assessment of viral virulence (via the analysis of cell-cell fusion activity) may overestimate the pathogenic potential of the tested variant.
While acknowledging their puzzlement about the origin of the often-remarkable number of mutations and significant changes in the biological functions of rapidly succeeding variants and lacking an explanation for why BA2.86 has lost the attenuation characteristics observed in most Omicron predecessors, such as inefficient infection of lung cells, many scientists draw scientifically unfounded conclusions regarding the source behind the never-ending series of newly emerging variants. Their ignorance of the adaptive immune mechanisms driving these mutations in highly C-19 vaccinated populations, coupled with the presence of similar mutations in other Omicron sublineages following prolonged amplification in immunocompromised patients, leads them to consider individuals with reduced immune function as a potential breeding ground for highly mutated SC-2 variants, such as Omicron BA.1 and BA.2.86.
However, considering the suboptimal population-level immune pressure on viral infectiousness, attributed to suboptimal cytotoxic T cell (CTL) activity following vaccine breakthrough infection (VBTI) with highly infectious Omicron descendants (https://www.voiceforscienceandsolidarity.org/scientific-blog/the-fulminant-spread-of-jn-1-is-a-highly-worrisome-prognostic-indicator), it is not surprising to observe productive infectiousness-enhancing mutations in viral proteins of BA.2.86/JN.1 other than the S protein (https://www.forbes.com/sites/williamhaseltine/2023/10/26/jn1-the-odd-man-out-among-omicron-sublineages/?sh=74aa039b3e47&s=03). The selection of these mutations could be interpreted as reflecting in vivo adaptation of the virus to the collective CTL-mediated immune pressure on viral infectiousness, enhancing its transmissibility and enabling newly emerging sublineages to substantially expand in prevalence. Additionally, VBTIs with highly infectious Omicron descendants result in a decrease in the production and/or an increase in the consumption of virulence-inhibiting PNNAbs (https://www.voiceforscienceandsolidarity.org/scientific-blog/scientists-molecular-stamp-collection-raises-false-hopes-on-outcome-of-c-19-pandemic). In line with the resulting suboptimal population-level immune pressure on viral virulence, it is not surprising to find that BA.2.86/JN.1 infects lung cells with heightened efficiency and exhibits a higher cell-cell fusion capacity in lung cells compared to previous Omicron descendants.
These altered biological characteristics and the selected underlying mutations are fully compatible with enhanced efficiency of trans infection and trans fusion (i.e., the fusion of infected with uninfected cells). They could be interpreted as reflecting natural selection of additional mutations promoting in vivo adaptation of the virus to the growing, suboptimal PNNAb-mediated immune pressure collectively exerted on viral virulence in highly C-19 vaccinated populations. Due to their enhanced capability to infect lung cells, BA 2.86/JN.1 would be more likely to cause severe disease in individuals whose PNNAb levels no longer suffice to sufficiently mitigate viral virulence. This likely contributes to the currently reported increase in hospitalization and death rates due to severe C-19 disease.
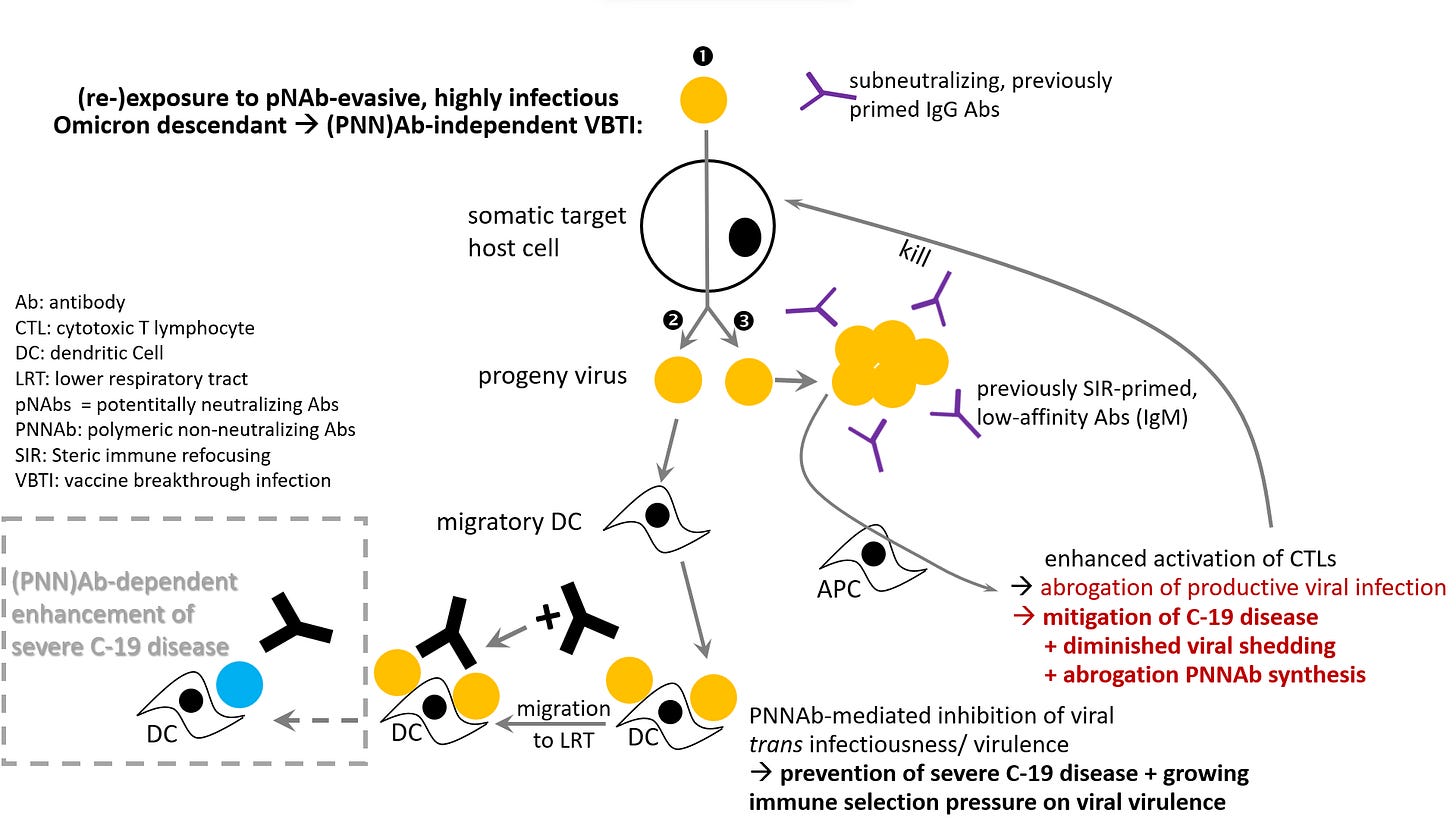
However, due to the enhanced viral uptake by antigen-presenting cells (APCs) in C-19 vaccinees, PNNAb levels will not decline rapidly enough in a sufficiently large portion of the population to widely release the brakes on PNNAb-mediated inhibition of viral trans infection. As a result, progeny virions adsorbed to migratory dendritic cells (DCs) would still be prevented from trans infecting lung cells in the majority of C-19 vaccinees (see fig. attached below). To overcome this hurdle, the virus will likely undergo a spectacular mutational change capable of collectively overriding PNNAb-mediated inhibition of trans infection, possibly in the form of a substantial change in the glycosylation profile of the S protein (https://www.voiceforscienceandsolidarity.org/scientific-blog/predictions-gvb-on-evolution-c-19-pandemic).
In conclusion, even though in vitro assessments of Omicron BA.2.86's biological traits suggest a potential for an increased capacity to spread and cause disease in the lower respiratory tract, it is reasonable to assume that the virulence-mitigating effect of PNNAbs currently continues to prevent a generalized increase in viral virulence in highly C-19 vaccinated populations. This will hold true as long as the population-level immune selection pressure exerted on viral virulence has not grown high enough to trigger a spectacular, virulence-enhancing change that would prevent the attachment of PNNAbs to the S-NTD (N-terminal domain of S protein) on DC-tethered virions.
In summary, the scientific community doesn't seem to grasp that the enhanced ability of BA2.86/JN.1 to efficiently enter lung cells via TMPRSS2-reliant plasma membrane fusion in vitro should be viewed as the precursor to yet another significant change in the S protein. This change could collectively trigger severe C-19 disease in highly C-19 vaccinated populations. It is difficult to imagine how and why such a dramatic alteration in the S protein, as I predict, would occur in a single immunocompromised individual—without widespread immune selection pressure on viral (trans) infectiousness. There is simply no reason to assume that the immune pressure exerted on a new variant that evolved in a single immunosuppressed person targets viral transmissibility. Immune pressure in an immunosuppressed person is likely to result from suboptimal cell-mediated immune responses targeting virus-infected cells rather than suboptimal antibody (Ab)-mediated responses targeting freely circulating virus. This is because the activation of cell-mediated immune responses, aimed at abrogating productive viral infection, precedes the priming of S-specific Abs meant to prevent viral entry. Given the high level of immune evasion toward neutralizing antibodies (NAbs) and other mutations promoting viral infectiousness or trans infectiousness, it is simply impossible for spectacular mutants such as Omicron BA.1 and Omicron BA2.86 to have emerged and spread as a result of immune pressure exerted by one or another immunosuppressed individual experiencing prolonged infection due to delayed virus clearance.
On the contrary, mutations underlying alterations in biological properties relevant to viral transmission have been shown to result from convergent evolution[1] across multiple lineages globally spreading in highly C-19 vaccinated populations, both in the pre-Omicron BA.1 and even more so in the post-Omicron BA.1-pre-Omicron BA.2.86 era (https://www.nature.com/articles/s41586-022-05644-7; https://pubmed.ncbi.nlm.nih.gov/37169744/). The authors of the first publication also concluded that the global pandemic indeed has greatly promoted the efficiency of the virus to evolve immune escape mutations. The most likely reason for distinct lineages to converge their evolving mutations to the same hotspots during a pandemic that cannot be controlled by large-scale vaccination is herd (i.e., population-level) immune pressure! There is no reason why Omicron BA.1 and Omicron BA.2.86 should be an exception to this rule.
I, therefore, have no choice but to conclude that:
i) there is no scientific basis for postulating that the unprecedented circulation of newly emerging variant variants during this pandemic resulted from immune selection and recombination within individuals with prolonged infections.
ii) There can be no doubt that vaccination of entire populations in the course of this pandemic has led these populations to exert collective immune pressure on viral infectiousness, and that this immune pressure has been perpetuated as a result of SIR (steric immune refocusing)-enabling VBTIs. This evolution will ultimately generate population-level immune pressure on viral trans infectiousness, leading to a potentially disastrous scenario. Therefore, the emergence and high transmissibility of JN.1 clan members represents a very worrisome evolution of the virus.
Suggesting that immunocompromised people could be a source of highly mutated viruses that could steer the trajectory of the pandemic in an ‘unexpected’ direction is not only unscientific but also irresponsible, as it provides the stakeholders of this mass vaccination with a cheap way out to shift an undesirable turn of this pandemic onto the shoulders of the most vulnerable in society.
As mentioned above, the authors’ hypothesis that the production of new variants which can enter target cells through the TMPRSS2-dependent pathway might reduce their transmission is not supported by valid experimental evidence. Regardless of whether reduced viral infectivity measured in vitro truly reflects BA.2.86 infectivity in vivo, the postulate that BA.2.86 might reduce viral transmission is irrelevant as it has become evident that all representatives of the JN.1 clan, including JN.1 itself (the closest descendant of BA.2.86) and its viral offspring, have significantly increased their ability to infect new hosts compared to BA.2.86 while sharing the same lung infecting properties and multiple infection-enhancing mutations in other viral proteins with BA.2.86. JN.1’s L455S FLip mutation[2] alone was sufficient to make the variant highly transmissible and rapidly predominant in several different countries, surpassing BA.2.86 and other co-circulating variants and reaching peak concentrations in wastewater.
Consequently, asserting that ‘No matter how virulent a variant is, it won’t cause much damage overall if it can’t successfully infect new hosts’ (https://www.salon.com/2024/01/12/more-severe-disease-symptoms/) is a void statement that lacks a basis in how the virus behaves in the field, specifically in highly C-19 vaccinated populations. As previously explained, these populations are now experiencing the weakening of their last line of immune defense (provided by the PNNAbs), essentially serving as a breeding ground for a spectacular set of mutations enabling the virus to collectively overcome PNNAb-mediated inhibition of viral virulence in highly C-19 vaccinated populations. In terms of science-based predictions on the current evolution of SC-2, the above statement should rather be replaced by “No matter how infectious a new variant is, it will cause much damage overall if it can no longer elicit a protective immune response[3].
Fig.: Newly emerged, highly infectious Omicron descendants do not rely on PNNAbs to infect target host cells (). Replication of highly infectious variants generates an immunological environment that promotes their adsorption onto tissue-resident DCs. PNNAbs bind in high quantities to progeny virus tethered to these DCs, which subsequently migrate to the lungs and other distal organs (). Diminished production of these virulence-inhibiting PNNAbs, combined with their enhanced binding to DC-tethered virions, leads to increasing immune selection pressure on viral virulence in highly C-19 vaccinated populations. As previously SIR-primed Abs bind with low-affinity to the highly infectious, antigenically more distant immune escape variant, large Ab-virus complexes are taken up into patrolling APCs (). Enhanced uptake of large Ab-virus complexes into APCs facilitates strong activation of CTLs, thereby enabling the elimination of virus-infected host while impeding T help to assist in boosting previously SIR-primed Abs. Diminished boosting of previously primed anti-S Abs results in diminished production of PNNAbs. As explained in the text, enhanced viral uptake by APCs will slow down the adsorption of highly infectious progeny virions on migratory DCs and thereby mitigate the decrease in PNNAb concentration resulting from diminished production. Hence, PNNAb levels may not decline rapidly enough in a sufficiently large portion of the population to widely release the brakes on PNNAb-mediated inhibition of viral trans infection. However, with more infectious BA.2.86 descendants (i.e., the JN.1 clan) emerging and rapidly growing in prevalence, highly C-19 vaccinated populations are exerting a steadily increasing immune selection pressure on viral virulence. This is thought to eventually trigger the selection of a new variant that has the capacity to cause highly virulent VBTIs in highly C-19-vaccinated populations due to PNNAb-dependent enhancement of severe C-19 disease.
[1] Convergent evolution implies that separate viral sublineages acquire similar or identical mutations, suggesting
limited evolutionary space of circulating SARS-CoV-2 lineages.
[2] L455S is nicknamed FLip mutation because the positions of two amino acids on the spike protein labelled L and S are switched. This mutation increases the immune evasiveness of JN.1 while enhancing its intrinsic infectiousness due to a stronger binding affinity between its receptor binding domain and ACE2.
[3] As previously explained, the failure to mount a successful/ effective immune response will ensue, with the innate immune system not being trained to handle high viral loads and the adaptive immune response, the special forces, being derailed to the point of becoming dysfunctional—resulting from immune refocusing.




Wow.... You have said this before but it is worth highlighting. "To overcome this hurdle, the virus will likely undergo a spectacular mutational change capable of collectively overriding PNNAb-mediated inhibition of trans infection, possibly in the form of a substantial change in the glycosylation profile of the S protein" I think the important word here is "overriding" rather than just evading. This variant will just bypass the only remaining immunity of a highly vaccinated person.
As a lay person, I don't fully grasp all of what Geert is telling us, but I am really, really worried by what I am seeing happening around me this winter here in Glasgow Scotland.
The number of people I know who have had multiple courses of antibiotics for ongoing lung infections is just ridiculous. One lady has had 6 courses of antibiotics spanning since November and she still isn't fully well, others have had multiple courses and prednisolone, and are waiting for chest x-rays... This is in the 25-65 age group. I have never ever heard of, or seen the like of this before. The GPs must know this is happening, they must see it in their surgeries.
Whatever is going on, it's not normal and it's very worrying. There is no herd immunity here, and people are not well.